Abstract

Children with sickle cell disease (SCD) have increased morbidity and mortality secondary to serious bacterial infections (SBI) by encapsulated organisms. These include bacteremia, acute chest syndrome (ACS), urinary tract infection, meningitis, osteomyelitis, septic arthritis, and cholangitis. For febrile patients with SCD, screening tools have been used in pediatric emergency departments (ED) across the United States. One such screening tool is a clinical pathway utilized at the Children's Hospital of Philadelphia, where low-risk criteria is used to determine risk for SBI and management thereafter (Ellison et al. Journal of Pediatric Hematology/Oncology 2018). Our institution defines low-risk criteria as lacking all of the following; ill-appearance, hypotension, a temperature ≥40 oC, history of Streptococcus pneumoniae bacteremia, diagnosis of ACS, clinical or laboratory concern for splenic sequestration (Hgb decrease by >2g/dL from baseline with an enlarging spleen and/or thrombocytopenia with platelets <100k/uL), white blood cell count >5k/uL and <30k/uL, Hgb <5g/dL, non-adherence with penicillin prophylaxis, cephalosporin allergy, incomplete immunizations, or concerns regarding appropriate follow up. Our institution routinely admits febrile patients, <24 months of age with SCD, irrespective of any other factor. Given the low rate of SBI among febrile children with SCD at low-risk, and the risks associated with hospital admissions, there is likely an opportunity to safely treat younger children similarly to their older counterparts.
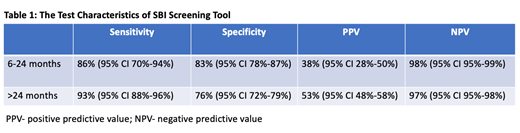
The primary objective of our study is to compare test characteristics, specifically the negative predictive value (NPV), of our screening tool (not including age) on predicting risk of SBI in febrile children with SCD ages 6-24 months and those older than 24 months.
This 10-year retrospective cohort study included patients with SCD <21 years old who had fever (≥38 oC, during their visit or on history prior to arrival) and were seen in the ED or Pediatric Hematology outpatient clinic at our institution. Test characteristics (sensitivity, specificity, positive predictive value (PPV) and NPV) of our screening tool were calculated for both age groups. Pearson's chi square was utilized to compare the test characteristics between the two groups.
A total of 1226 encounters were analyzed, 320 (26%) of those were patients 6-24 months of age and 877 (72%) of those were patients >24 months. There were 35 (11%) patients in the 6-24 month cohort that had an SBI and 201 (23%) patients in the >24 month cohort that had an SBI. The sensitivity, specificity, PPV and NPV for both age cohorts are represented in Table 1. There was no statistically significant difference between the NPV of those 6-24 months of age 98% (95% CI 95%-99%) and the NPV of those >24 months of age 97% (95% CI 95%-98%) with a p-value of 0.63.
In conclusion, the screening tool performed well in identifying children with SCD and fever who are at low-risk of SBI in both age ranges. There was no difference in its performance in the younger group suggesting that a cut-off age of 2 years is not an independent risk factor for SBI and that children 6-24 months should not be admitted solely because of their age.
No relevant conflicts of interest to declare.
Author notes
 This icon denotes a clinically relevant abstract
This icon denotes a clinically relevant abstract